QUICK LINKS: Practice Support Tools | Patients | Find a Neuro-Ophthalmologist | NOVEL | YONO Portal | Our Journal | Fellowships
Non-Arteritic Anterior Ischemic Optic Neuropathy
Patients: Download as pdf
Clinicians: Download as pdf
NEW RESOURCE! Semaglutide And NAION Brochure
What is non-arteritic anterior ischemic optic neuropathy?
Non-arteritic anterior ischemic optic neuropathy (NAION or NA-AION) is caused by decreased blood flow to the front part of the optic nerve (optic disc). It causes optic nerve swelling and sudden vision loss. NAION typically affects one eye, although the other eye sometimes suffers similar loss months or years later (there is about a 15% risk of second eye involvement within 5 years). Rarely, both eyes may be affected at the same time.
The blood supply to the front of the optic nerve comes from small branches off the ophthalmic artery, which comes off of the carotid artery. Loss of the blood supply within those small branches damages the front part of the optic nerve, causing it to swell and resulting in vision loss. The swelling eventually goes away, but part of the optic nerve is permanently damaged.
Why does the optic nerve lose blood flow in NAION?
We do not completely understand the cause of the loss of blood supply to the optic nerve. We do know that it happens more often in patients born with small optic discs (the front part of the optic nerve that can be seen within the eye). This crowded optic disc structure (often referred to as a small cup-to-disc ratio or a “disc at risk”) makes the nerve more vulnerable to blood supply problems. Some researchers have suggested that transient fluctuations in blood pressure may play a role in the onset of NAION, but this is controversial. Other risk factors may include the chronic vascular effects of:
- Smoking
- Diabetes
- High blood pressure
- Sleep apnea
- Anemia
- Kidney disease
Certain drugs used for erectile dysfunction such as sildenafil (Viagra), vardenafil (Levitra) and tadalafil (Cialis or Adcirda) may be associated with NAION and should be avoided after NAION occurs. The heart medication amiodarone may predispose to NAION and should be stopped after NAION, if possible. Your doctor should discuss this with your cardiologist before any changes are made to your heart medications.
In most cases, nothing you did or did not do caused NAION.
How does NAION affect my eyes and vision?
Most people with NAION experience sudden painless vision loss in one eye. The vision loss often consists of a gray or dark spot that does not move or change or a severe blur. For many people, the vision loss affects the bottom or top half of the vision in one eye, although other patterns of vision loss may occur.
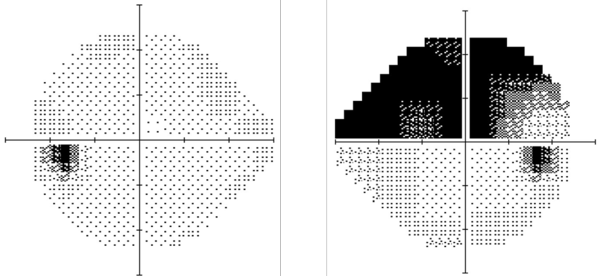
Left Eye | Right Eye
Visual field test of a NAION patient: This test is done in the doctor’s office to assess the peripheral vision. These images represent the peripheral visual fields from the patient’s perspective. The darker area seen in the upper part of the figure in the right eye represents peripheral visual loss involving the top half of vision in the right eye. The left eye is normal.
Your eye doctor may describe your optic nerve as swollen. A normal optic nerve is orange in color, has sharp, distinct margins, and is flat; when there is decreased blood flow to the optic nerve, the optic nerve swells.
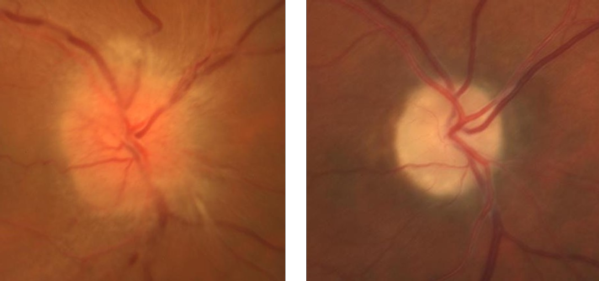
Left: Optic disc swelling in right eye from NAION | Right: Optic disc atrophy of the same eye 3 months later
Why do I need to see a neuro-ophthalmologist?
A neuro-ophthalmologist is a medical doctor whose specialty includes the optic nerve. The diagnosis of NAION is a clinical one, meaning that there is no one test that gives us the diagnosis. A number of features are taken into consideration. Neuro-ophthalmologists are experts at making this clinical judgment.
The neuro-ophthalmologist will evaluate your vision and may perform or order additional tests to rule out other causes of optic nerve swelling and vision loss. Visual acuity measures the sharpness of your central vision (ability to read the eye chart). Color vision is tested using figures or numbers composed of colored dots. A visual field test maps your field of vision, sometimes called your side or peripheral vision. The response of the pupil to a bright light is assessed. Additional tests measure the thickness of the optic nerve fibers.
What non-visual tests might my doctor order?
Your doctor may recommend testing to assess the risk factors for NAION such as measuring blood pressure and obtaining blood tests for diabetes and high cholesterol. Tests, such as MRI scan of the brain and orbits, are sometimes ordered to rule out other potential causes of vision loss from optic nerve damage.
A specific kind of inflammation, called giant cell arteritis, can cause vision loss very similar to NAION (arteritic anterior ischemic optic neuropathy). To check for this disease, your doctor may ask you about other symptoms, order blood tests and perform a biopsy of a scalp artery.
What will happen to my vision? What is my prognosis?
- Most people with NAION do not lose further vision in the affected eye after the initial vision loss. However, about up to one-third of people will lose additional vision during the first weeks while the optic nerve is still swollen. If your vision continues to worsen over more than a few weeks, contact your doctor.
- The optic nerve swelling goes away by 1-2 months, leaving behind permanent changes to the optic nerve and to your vision.
- Around 40% of people with significant visual acuity loss from NAION have some improvement in central vision over time. Unfortunately, the area of visual field loss does not usually improve. It may, however, become less noticeable with time, especially if the other eye is normal.
- Your other eye may develop NAION in the future. Approximately 15% of people with NAION in one eye will develop NAION in the other eye within 5 years. Diabetes may increase your risk of developing NAION in the other eye. If you have obstructive sleep apnea, compliance with your CPAP machine may help reduce the chance of a second attack. Your doctor will likely recommend a sleep study if you do not already have a diagnosis of sleep apnea.
- A repeat attack of NAION in the same eye is rare.
What treatments are available for NAION?
Unfortunately, there is no proven effective treatment for NAION. Many research studies have looked at different medications and surgical operations to treat NAION with no measurable effect on vision. Likewise, there is no proven preventive treatment at this time. Despite this, many neuro-ophthalmologists recommend some medical treatments and basic steps for your health:
- Talk with your primary care provider about the risk factors that can affect NAION. Screening for diabetes, high cholesterol, high blood pressure, and sleep apnea are important for your overall health.
- While chronic high blood pressure is a risk factor for NAION, it is also important that your blood pressure not run too low.
- Some neuro-ophthalmologists will treat patients with very recent visual loss or worsening visual loss from NAION with oral steroids for a few weeks. Other neuro-ophthalmologists worry that the negative effects from the steroids outweigh the potential benefits.
- Many neuro-ophthalmologists recommend taking daily aspirin with the hope of reducing the risk of the other eye becoming involved, although it is uncertain this helps. Aspirin reduces the risk of heart attacks and strokes, which can also occur in people with NAION.
- If you smoke, you should work with your primary care provider to stop smoking.
- If you take erectile dysfunction medications or amiodarone, please let your doctor know, as these agents can sometimes be associated with NAION.
- Your doctor may recommend a sleep study to check for sleep apnea. There is some evidence that the risk of second eye involvement may be higher in patients with untreated sleep apnea.
Copyright © 2023. North American Neuro-Ophthalmology Society. All rights reserved.
This information was developed collaboratively by the Patient Information Committee of the North American Neuro-Ophthalmology Society. This has been written by neuro-ophthalmologists and has been edited, updated, and peer-reviewed by multiple neuro-ophthalmologists. The views expressed in this brochure are of the contributors and not their employers or other organizations. Please note we have made every effort to ensure the content of this is correct at time of publication, but remember that information about the condition and drugs may change. Major revisions are performed on a periodic basis.
This information is produced and made available “as is” without warranty and for informational and educational purposes only and do not constitute, and should not be used as a substitute for, medical advice, diagnosis, or treatment. Patients and other members of the general public should always seek the advice of a physician or other qualified healthcare professional regarding personal health or medical conditions.









_200x72(1).png)