QUICK LINKS: Practice Support Tools | Patients | Find a Neuro-Ophthalmologist | NOVEL | YONO Portal | Our Journal | Fellowships
Myasthenia Gravis
Patients: Download as PDF
Clinicians: Download as PDF
What is myasthenia gravis?
Myasthenia gravis (MG) is an autoimmune disease in which the body's immune system creates antibodies (proteins that normally protect us) that may attack receptors on your muscles. This results in muscle weakness because the muscles do not receive the signals to contract (tighten). Muscles anywhere within the body may be affected. In ocular MG, eyelid droop (ptosis) and double vision may occur if the muscles that control the eyelids and eye movements are affected. In generalized MG, muscles of the eyes, limbs, neck, as well as muscles of speaking, swallowing or breathing may also be involved. Patients with ocular MG can develop generalized MG over time so it is important to monitor closely.
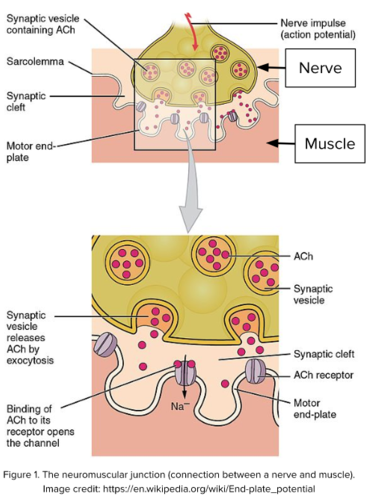
How are the nerves and muscles affected in myasthenia gravis?
- When you want to move a muscle, the brain sends a signal through the nerves that go to the muscle. At the junction between the nerve and muscle, the nerve ending releases a chemical called acetylcholine (ACh) that travels from the nerve to the muscle. The space between the nerve and the muscle is called the synapse or the neuromuscular junction.
- On the muscle side of the synapse, there are receptors that are waiting to detect acetylcholine. When acetylcholine connects with them, the muscle contracts.
- In MG, acetylcholine is released normally, but antibodies produced by the body’s immune system block and eventually damage the acetylcholine receptors on the muscle side. The muscle may work at first, but the signal weakens more quickly than normal and, over time, repeated movement may result in a gradual increase in weakness. Muscles that are used frequently are most likely to be weak.
How can myasthenia gravis affect me?
Many people with MG only have eye symptoms (“ocular myasthenia gravis”). These patients have weakness of the muscles that open the eyelids and/or the muscles that move the eyes. This weakness results in lid droop (ptosis) and double vision due to variation in weakness of different eye muscles between the two eyes. The double vision goes away if you close either eye.
MG can affect other muscles in the body (“generalized myasthenia gravis”). Shortness of breath or difficulty swallowing are more serious symptoms of MG and must be brought to your doctor's attention immediately as they can be life-threatening.
MG does not produce pain or numbness, vision loss or a change in the size of your pupil. If these are present, they may be due to another process, and you should inform your doctor.
Why do I need to see a neuro-ophthalmologist?
A neuro-ophthalmologist specializes in neurological problems related to the eyes and eye movements. They are often involved in diagnosing myasthenia gravis, especially if the eyelids are droopy or if you have double vision.
There are many different ways myasthenia gravis is diagnosed. Your doctor may diagnose you in the clinic, but may order blood tests or other special tests to help confirm the diagnosis.
- A blood test for antibodies can help confirm the diagnosis, but the antibodies are not always detectable, especially if you only have ocular myasthenia gravis.
- Your doctor may perform tests in the office to see if there is improvement of your eyelid drooping. One example is the ice test, where your doctor places an ice pack on your eyelids for several minutes, then re-examines your eyelids to see if there is any improvement. In the rest test, the doctor may ask you to close your eyes for 20 minutes to see if that leads to improvement. If the diagnosis remains unclear, you may be sent to a neurologist with special training in neuromuscular disease who can perform a nerve conduction test (NCT) or electromyogram (EMG) which are tests that look at the nerve signals and muscle activity for signs of MG.
- Once you have been diagnosed with myasthenia gravis, your doctor may order additional testing and refer you to a general neurologist (or a neurologist specializing in neuromuscular diseases) for further treatment. There have been several recent advances in the treatment of myasthenia gravis.
Example of Ice Test
Before Ice

After ice

What is my prognosis?
As with other autoimmune diseases, the symptoms of myasthenia gravis tend to fluctuate. MG produces variable disease that may last for years or indefinitely. Symptoms may suddenly become worse. They may be triggered by some medications, so you should ensure that your doctor has an updated list of all of your medications, including supplements (see below). Once the diagnosis of MG is made, patients need to inform all their physicians of their diagnosis, particularly if they are ever seen in an Emergency Department or are scheduled for any type of surgery with anesthesia.
How is myasthenia gravis treated?
- Myasthenia gravis can be treated with pyridostigmine (Mestinon), a medication that helps with the symptoms of muscle weakness. Unfortunately, this does not always relieve lid drooping or double vision.
- Steroid medication may also improve muscle function by affecting the immune system’s ability to produce antibodies. Steroids can have many side effects. If your immune system needs to be treated long-term, your doctor will help determine whether to use steroids or other medications that affect immune function.
- Other medications they might use include intravenous immunoglobulin (IVIg), Azathioprine (Imuran), Mycophenolate mofetil (Cellcept) or Rituximab (Rituxan). For generalized MG, there are currently 3 FDA-approved medications including Eculizumab (Soliris), Ravulizumab (Ultomiris) and Efgartigimod alfa (Vyvgart) that may also be used.
- Occasionally surgery to remove the thymus gland may be effective at treating MG. Your doctor may check for thymus enlargement with a chest CT scan.
Is there a cure for myasthenia gravis?
At this time, there is no known cure for myasthenia gravis. However, many patients are able to control their symptoms with medication alone and the severity of the disease may improve over time.
What are my chances of developing weakness in muscles other than my eye muscles?
Myasthenia gravis can affect many muscles or only a few muscles, especially the muscles that move the eye and lift the lid. The chance that ocular MG will involve muscles in the rest of your body is decreased after two years, but there is still a small risk of other muscles becoming affected. Inform your physician immediately if you develop problems with breathing or swallowing.
I have myasthenia gravis. What if I become pregnant?
If you have myasthenia gravis and become pregnant, please talk with your doctor to make sure that both you and the baby do well. Myasthenia gravis does not increase risk of miscarriage or affect the fetus during pregnancy. Myasthenia gravis can worsen during pregnancy, and extra care is typically needed during delivery. After birth, the baby may have some weakness related to the antibodies from the mother, but that usually gets better on its own. If you notice your baby has difficulty feeding or breathing, please talk with your doctor.
Are there medications that can make myasthenia gravis worse?
There are many medications that may trigger myasthenia gravis symptoms or make myasthenia gravis worse, such as some antibiotics and some blood pressure and cholesterol medications. Please talk with your doctor about your medications. A partial list can be found at: https://myasthenia.org/What-is-MG/MG-Management/Cautionary-Drugs
What are some support groups for myasthenia gravis?
Here is a partial list of foundations and support groups:
- Myasthenia Gravis Foundation of America: https://myasthenia.org
- Myasthenia Gravis Hope Foundation: https://mghope.org
- Neuro Talk Support Group: https://www.neurotalk.org/myasthenia-gravis/
Copyright © 2023. North American Neuro-Ophthalmology Society. All rights reserved.
This information was developed collaboratively by the Patient Information Committee of the North American Neuro-Ophthalmology Society. This has been written by neuro-ophthalmologists and has been edited, updated, and peer-reviewed by multiple neuro-ophthalmologists. The views expressed in this brochure are of the contributors and not their employers or other organizations. Please note we have made every effort to ensure the content of this is correct at time of publication, but remember that information about the condition and drugs may change. Major revisions are performed on a periodic basis.
This information is produced and made available “as is” without warranty and for informational and educational purposes only and do not constitute, and should not be used as a substitute for, medical advice, diagnosis, or treatment. Patients and other members of the general public should always seek the advice of a physician or other qualified healthcare professional regarding personal health or medical conditions.









_200x72(1).png)