QUICK LINKS: Practice Support Tools | Patients | Find a Neuro-Ophthalmologist | NOVEL | YONO Portal | Our Journal | Fellowships
Thyroid Eye Disease
Patients: Download as PDF
Clinicians: Download as PDF

Courtesy of American Academy of Ophthalmology and Dr. Steven A. Newman, M.D.
What is thyroid eye disease?
Thyroid eye disease (TED) or thyroid related ophthalmopathy (TRO) is an autoimmune condition in which your body's immune system triggers inflammation in the eye socket (also called the orbit), affecting the muscles that move the eye and the fatty tissue behind the eye. The disease can cause the eyes to bulge forward (proptosis), the eyelids to open more so it looks like you are staring (eyelid retraction), double vision, decreased vision, red eyelids and eye irritation. Rarely, it can cause pressure on the optic nerve (the nerve that connects the eye to the brain) causing vision loss or an ulcer of the cornea, the clear front part of the eye, causing pain.
The immune system normally produces antibodies to fight infections. In autoimmune diseases, the immune system gets misdirected and produces antibodies that instead attack parts of the body such as the eye sockets, producing inflammation. The antibodies that cause thyroid eye disease often attack the thyroid as well, causing abnormal thyroid function, but in some cases, the thyroid hormone levels are normal. When the antibodies increase thyroid function, it is called Graves’ Disease, and when the antibodies decrease thyroid function, it is called Hashimoto’s Disease.
Too much thyroid hormone causes:
- Shaking
- Weight loss
- Rapid or irregular heartbeat
- Nervousness/anxiety
- Sweating
Not enough thyroid hormone causes:
- Fatigue
- Sensitivity to cold
- Weight gain
- Hair loss
- Constipation
How does thyroid eye disease affect my eyes?
The appearance of the eyes and eyelids in a patient with thyroid eye disease. Note the eyelid retraction (upper lid elevation) and protrusion of the eyes (proptosis), eyelid swelling, and redness of the eyes.
- The antibodies that attack the thyroid gland can also attack the fat and muscles around the eye. This attack can happen even if your thyroid levels are normal.
Thyroid eye disease affects the eyes in many ways, including the following:
- Eyelid retraction, when e eyelids gets pulled backward, exposing more of the eye
- Protrusion or bulging of the eye forward (proptosis)
- Eyelid swelling
- Blurred or distorted vision
- Dry eyes
- Double vision: the muscles that move the eyes may swell and scar. When this happens, the eyes do not move as well and point in different directions, causing misalignment of the eyes and double vision. Closing one eye will make this kind of double vision go away.
- Optic nerve damage: if the muscles swell too much, they can press on the optic nerve, resulting in vision loss. This complication is rare (around 5%) and may be reversible when treated rapidly.
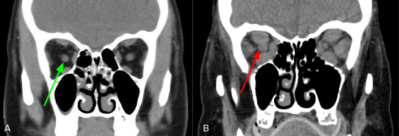
A. Modified from Radiopaedia.org. Case courtesy of Dr. Dalia Ibrahim. rID: 44049. B. Courtesy of Dr. Nagham Al-Zubidi.
CT scan of the orbit.
A. Normal eye. The optic nerve (green arrow) is surrounded by normal eye muscles (gray ovals).
B. Thyroid eye disease. The eye muscles (gray ovals) are enlarged with compression of the optic nerve (red arrow).
What is the prognosis of thyroid eye disease?
Thyroid eye disease often comes and goes. The inflammation of the orbit can last for 6 months to a few years (active phase) before it calms down (inactive phase). The effects on your eyes may become permanent, especially if untreated.
Even after the inflammation resolves, the eyes often do not return to their prior appearance. Cigarette smoking (as well as second-hand smoke) worsens the severity and prolongs the active phase of thyroid eye disease.
How is thyroid eye disease treated?
The goal of thyroid eye disease treatment is to decrease the symptoms and severity of orbital involvement. Avoiding tobacco smoking and returning thyroid hormone levels to normal decrease the severity of eye involvement. Treatment is most effective early in the active phase.
Your doctors, including your primary care provider and endocrinologist, will work with you on controlling your thyroid hormone levels.
- High thyroid hormone levels: you may be treated with medications, radioactive iodine, or thyroid surgery.
- Low thyroid hormone levels: you will need to take hormone replacement medication.
Other important factors that help with treatment are:
- Smoking cessation
- Artificial tear solution during the day and lubricating ophthalmic ointment at night
- Taping the eyelids closed at night if the eyelids are not closing completely
- Humidifiers, moisture chamber goggles/glasses and punctal plugs (small plugs that go into the tear drainage system in the lower lids and increase natural tears)
- Supplementation with a natural mineral called selenium.
Double vision treatments include:
- Temporary prism glasses to shift the images to give you single vision
- Covering one eye (either eye may be covered)
- Eye muscle surgery
Treatments for decreasing inflammation around the eye include:
- Steroids such as prednisone
- Low-dose radiation can lessen inflammation during the active phase of the disease.
Occasionally, surgery may be necessary to treat your symptoms:
- Orbital decompression surgery creates room in the eye socket by removing some of the bones of the eye socket, removing some of the fatty tissue in the eye socket, or both.
- Eye muscle surgery helps correct double vision.
- Eyelid surgery helps to restore the eyelids to a normal position.
What new treatments are available for thyroid eye disease?
Teprotumumab is an injected medication that targets one of the triggers for inflammation in thyroid eye disease. Teprotumumab (Tepezza; Horizon Therapeutics plc), a drug evaluated in the OPTIC and OPTIC-X trials, has been shown to improve symptoms of thyroid eye disease such as eye bulging and double vision in the active phase by decreasing inflammation and swelling behind the eye. Possible side effects include muscle cramps, increased blood sugar, hair loss and hearing loss. It is a new treatment and has not yet been studied for all cases of thyroid eye disease. In January 2020, the FDA approved teprotumumab for the treatment of thyroid eye disease in the United States. Talk with your doctor to see if you would be a candidate for this treatment.
Additional Reading/Resources
- Thyroid Eye Disease
- American Thyroid Association
- International Thyroid Eye Disease Society
Support Groups
- https://www.thyroideyes.com/thyroid-eye-disease-support/ted-and-vision-support-groups
- https://www.facebook.com/ThyroidEyes
- https://www.facebook.com/SER4ThyroidPage
Copyright © 2023. North American Neuro-Ophthalmology Society. All rights reserved.
This information was developed collaboratively by the Patient Information Committee of the North American Neuro-Ophthalmology Society. This has been written by neuro-ophthalmologists and has been edited, updated, and peer-reviewed by multiple neuro-ophthalmologists. The views expressed in this brochure are of the contributors and not their employers or other organizations. Please note we have made every effort to ensure the content of this is correct at time of publication, but remember that information about the condition and drugs may change. Major revisions are performed on a periodic basis.
This information is produced and made available “as is” without warranty and for informational and educational purposes only and do not constitute, and should not be used as a substitute for, medical advice, diagnosis, or treatment. Patients and other members of the general public should always seek the advice of a physician or other qualified healthcare professional regarding personal health or medical conditions.










_200x72.png)
.png)