QUICK LINKS: Practice Support Tools | Patients | Find a Neuro-Ophthalmologist | NOVEL | YONO Portal | Our Journal | Fellowships
Pituitary Tumor
Patients: Download as PDF
Clinicians: Download as PDF
What is a pituitary tumor?
The pituitary gland is a pea-sized gland that sits underneath the base of the brain. It produces and releases many hormones. These hormones control your metabolism, stress level, growth, ovulation and menstruation in women, sperm and testosterone production in men, milk production, and urine production. Because of its many functions, it is often referred to as the “master gland.”

A pituitary adenoma is a common non-cancerous overgrowth (tumor) of the pituitary gland. Some pituitary adenomas cause changes in your hormone levels. Many are very small (microadenomas). Some grow very large (macroadenomas) and may push on the vision pathways. Many people who have pituitary adenomas may not have any symptoms and don’t realize they have one, especially because the vision loss may occur slowly over a long period of time.
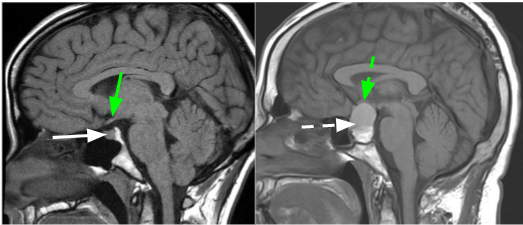
Left: Modified from Radiopaedia.org. Case courtesy of Dr. Frank Gaillard. rID: 17529. | Right: Courtesy of Dr. Kevin E. Lai, M.D.
MRI images showing the normal pituitary gland (solid white arrow) and a pituitary tumor (dashed white arrow). The optic chiasm (where the optic nerves meet) is shown by the green arrows and is pushed up by the pituitary tumor.
How does a pituitary tumor affect me?
- Pituitary tumors may present with vision changes, headaches, weight gain, menstrual irregularities, lactation, impotence, and change in the bone structure in your face and hands. Other uncommon symptoms like double vision, abnormal eye movements, a large pupil or droopy eyelids may rarely occur. Many pituitary tumors do not cause any symptoms and are found incidentally on MRI.
- The optic nerves meet behind the eye at the optic chiasm.
- Because the optic chiasm sits on top of the pituitary gland, a large pituitary tumor can push on the optic nerves or chiasm and cause vision loss.
- Your peripheral vision is typically affected, but you may also lose central vision and color vision in one eye (if the optic nerve is compressed). Unfortunately, the vision loss can become permanent and this may limit your ability to drive or do other daily activities.
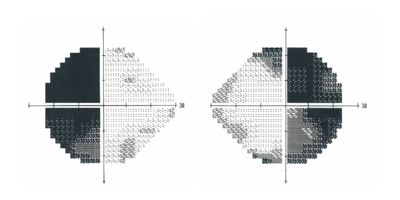
Left Eye | Right Eye Left Eye | Right Eye
Courtesy of Dr. Kevin E. Lai, M.D.
Peripheral (side) vision loss from a pituitary tumor. These pictures show vision in the left eye on the left and right eye on the right, both from the perspective of the patient. A. Normal visual fields where vision is preserved in both halves of each eye. B. Vision loss from compression by a pituitary tumor. The left half of the vision in the left eye and the right half of the vision in the right eye are dark and not seen.
- A hormone specialist (endocrinologist) helps evaluate hormone levels.
- Sometimes pituitary tumors cause low hormone levels (hypopituitarism), which may make you feel ill, feverish, sluggish, or fatigued.
- Sometimes pituitary tumors lead to an elevation in a hormone called prolactin which can result in enlargement of breast tissue and milk from the nipples. Sometimes pituitary tumors can cause elevation of growth hormone which can lead to an abnormal increase in the size of the feet, hands and head, and cause changes in facial appearance.
- A rare, but urgent condition caused by rapid bleeding into the tumor is known as pituitary apoplexy. People with pituitary apoplexy develop a sudden, severe headache, often with double vision or blurred vision, and may also feel feverish or have flu-like symptoms. This may also lead to lightheadedness from very low blood pressure. If you develop these symptoms, you should call your doctor or go directly to the emergency department. Rarely, this can also occur in pregnant women or those who have just given birth.
Why do I need to see an ophthalmologist or a neuro-ophthalmologist?
Because pituitary tumors affect many systems in your body, you may need to have different specialists who will help coordinate the best care for you.
- An ophthalmologist or neuro-ophthalmologist checks your central and peripheral vision, color vision and eye movements and may order some images.
- An endocrinologist monitors your hormones and treats any hormonal imbalances, and may use medicine to treat your tumor.
- A neurologist may monitor the tumor and treat the headaches.
- A neurosurgeon may need to perform surgery to treat the tumor.
- A radiation oncologist may use radiation to treat your tumor.
To help measure your vision, your doctor may perform several tests. The visual acuity test measures the sharpness of your central vision (ability to read the eye chart). Color vision can be tested using various plates with figures or numbers on them. A visual field test maps your field of vision. Other tests may also help your doctor look for changes in your optic nerves due to pressure on them from the tumor.
A CT scan or, preferably an MRI scan can help measure the size of the tumor and determine how close it is to your optic nerves, optic chiasm and other parts of your brain.
How are pituitary tumors treated?
Not all tumors need to be treated! Small tumors that do not cause any symptoms may be monitored without treatment.
- Hormonal imbalances are treated with medications prescribed by your endocrinologist.
- Some types of pituitary tumors can be treated with medications alone (especially prolactin-secreting tumors).
- Surgery (performed by a neurosurgeon) may be needed if the tumor can’t be treated with medication and is causing symptoms. The goal of surgery is to reduce the size of the tumor (debulking). Because surgery will likely affect how your pituitary gland works, you may need hormone replacement. Most often, removal of pituitary tumors can be performed through the nose, which can reduce recovery time following the surgery.
- In some cases, radiation therapy may be used to “kill” or control tumor cells. If the pituitary tumor is pressing on the optic nerve, focal radiation (focused on one spot) usually is not used, as it could damage the optic nerves. Because radiation therapy may affect how your pituitary gland works, you may need hormone medications after being treated. Radiation is used to prevent further growth of the tumor, and usually doesn’t shrink it much.
- People with pituitary apoplexy may need to be admitted to the hospital for close monitoring, hormone or steroid treatments, or surgery.
What is my prognosis? Will my vision get better?
Pituitary tumors are typically benign (non-cancerous) and slow growing. The longer you have vision loss, the less likely your vision will improve with treatment. However, even when there are signs of permanent damage to the optic nerves, there can still be good visual recovery if the pressure on the optic nerves is relieved with medication and/or surgery.
How often do I need to be examined?
How often your ophthalmologist or neuro-ophthalmologist needs to see you in follow-up will depend on your vision, how quickly it has changed in the past and MRI scan results. Your eye doctor may also examine you before and after any treatments. Once your vision is stable, you and your doctor may choose to extend the duration between your follow-up appointments.
Because pituitary tumors continue to grow slowly, even after a successful surgery, the tumor may come back. To help monitor the tumor, a brain scan (typically an MRI) should be performed on a regular basis. How often you need to be checked is different for everyone and should be discussed with your doctors.
Additional Reading/Resources
Other Websites
- Pituitary Tumor, by the National Library of Medicine on MedlinePlus (https://www.nlm.nih.gov/medlineplus/ency/article/000704.htm)
- This article from the U.S. National Library of Medicine is short but provides a lot of useful information about pituitary tumors. It also contains a video about the pituitary gland and how various hormones affect the body.
- Pituitary Tumors, by the Mayo Clinic (http://www.mayoclinic.org/diseases-conditions/pituitary-tumors/basics/definition/con-20028814)
- The Mayo Clinic has a web article about pituitary tumors geared towards patients.
- Pituitary Tumors, by The American Cancer Society (http://www.cancer.org/cancer/pituitarytumors/)
Support Groups
A list is found at the Johns Hopkins Neurology and Neurosurgery Pituitary Tumor page (http://www.hopkinsmedicine.org/neurology_neurosurgery/centers_clinics/pituitary_center/patient/support-groups.html).
- The Pituitary Network Association (http://pituitary.org)
- This is an international non-profit organization founded by people with acromegaly whose mission is to provide support for people with pituitary tumors and promote awareness and advocacy for pursuing treatments and cures for pituitary tumors.
- The National Brain Tumor Society (http://www.braintumor.org/)
- The National Brain Tumor Society serves as an advocacy group that raises money for awareness and research into various brain tumors. Their website has some helpful information about different brain tumors, as well as getting involved in support groups and contributing to brain tumor research.
- The Hormone Health Network (http://www.hormone.org/)
- The Hormone Health Network has handouts describing the different hormonal imbalances that can occur with pituitary tumors. They also have links to various support groups, depending on the hormone condition.
Copyright © 2023. North American Neuro-Ophthalmology Society. All rights reserved.
This information was developed collaboratively by the Patient Information Committee of the North American Neuro-Ophthalmology Society. This has been written by neuro-ophthalmologists and has been edited, updated, and peer-reviewed by multiple neuro-ophthalmologists. The views expressed in this brochure are of the contributors and not their employers or other organizations. Please note we have made every effort to ensure the content of this is correct at time of publication, but remember that information about the condition and drugs may change. Major revisions are performed on a periodic basis.
This information is produced and made available “as is” without warranty and for informational and educational purposes only and do not constitute, and should not be used as a substitute for, medical advice, diagnosis, or treatment. Patients and other members of the general public should always seek the advice of a physician or other qualified healthcare professional regarding personal health or medical conditions.









_200x72(1).png)
_200x72.png)