QUICK LINKS: Practice Support Tools | Patients | Find a Neuro-Ophthalmologist | NOVEL | YONO Portal | Our Journal | Fellowships
Optic Disc Drusen
Patients: Download as pdf
Clinicians: Download as pdf
What are optic disc drusen?
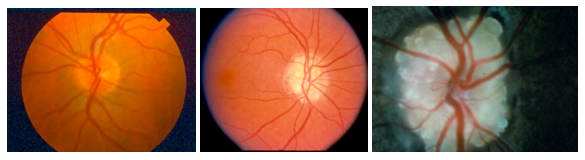
Optic disc drusen (ODD) are abnormal deposits of benign, usually calcified material within the optic disc, which is the front part of the optic nerve that connects each eye to the brain. We do not know the exact cause of optic disc drusen. They are present in 0.3-2% of people as an isolated case or they may run in some families (inherited). In children, they often are deep in the optic disc and hard to see (buried). Over time, they become more apparent as they enlarge and move closer to the surface of the optic nerve.
Optic disc drusen can look like swelling (edema) of the optic nerve. Papilledema is the medical term for swelling of the optic nerve from high pressure inside the head. Pseudopapilledema is the term for when the optic nerves look swollen but are actually not, and optic disc drusen are a leading cause of pseudopapilledema. True papilledema, which often presents with symptoms such as frequent/severe headaches, can be a dangerous condition that can be a sign of a brain tumor or other serious problem, and papilledema can lead to major vision loss. In contrast, optic disc drusen and other kinds of pseudopapilledema typically cause no symptoms and are not a sign of a brain tumor or another dangerous problem.
How do optic disc drusen affect me?
Patients with optic disc drusen usually do not notice any vision problems. Occasionally, patients may have flickering or graying out of vision that lasts a few seconds, or they may notice missing areas of vision. Over time, up to 70% of patients with optic disc drusen may develop some decrease in peripheral vision, which is typically mild. Visual field testing (called perimetry) is used to check the peripheral vision and follow-up on any abnormalities observed in the testing.
Because optic disc drusen can make the optic nerve appear swollen, patients with known optic disc drusen should inform any doctor examining their eyes of this condition to help avoid unnecessary alarm and testing.
Although optic disc drusen contain calcium, they are not generally associated with problems with calcium in the body, or with kidney or gallstones.
Why do I need to see a neuro-ophthalmologist?
A neuro-ophthalmologist is an optic nerve specialist. Neuro-ophthalmologists are experienced and trained in deciding whether an optic nerve looks swollen from optic disc drusen or from other causes to avoid unnecessary worry and testing. Different non-invasive tests may be used to evaluate your optic nerve to look for optic disc drusen, such as autofluorescent photography, ultrasound and/or optical coherence tomography (OCT). Visual field tests are done to detect and monitor any effects on visual function. In some cases, your doctor may obtain a fluorescein angiogram (FA) in which a dye called fluorescein is injected through a small IV to better rule out true optic disc swelling.
The examination also includes checking the pressure inside the eye (intraocular pressure, IOP). When patients with optic disc drusen are found to have elevated eye pressure they are typically treated with eye drops to lower the pressure because the high eye pressure and ODD can cause more peripheral vision loss.
Rarely, abnormal blood vessels related to optic disc drusen may form and cause vision problems. Early detection and treatment of the abnormal blood vessels can reduce the effects on vision. Very rarely, ODD can lead to a blockage in the arteries that feed the optic nerve, causing acute vision loss; this is called “nonarteritic anterior ischemic optic neuropathy” or NAION. Optic disc drusen can make diagnosing diseases that affect the optic nerve more difficult, and a neuro-ophthalmologist will look for signs of any such diseases.
Are there treatments for optic disc drusen?
There is no proven treatment for drusen, and there is no proven way to prevent the optic disc drusen from increasing in size. Once you have been diagnosed with optic disc drusen, your neuro-ophthalmologist or your regular eye doctor typically monitors your eyes periodically to look for any potentially related problems.
Resources
-
American Association for Pediatric Ophthalmology & Strabismus
https://aapos.org/glossary/optic-nerve-drusen -
American Academy of Ophthalmology
https://www.aao.org/eye-health/diseases/drusen-list
Copyright © 2023. North American Neuro-Ophthalmology Society. All rights reserved.
This information was developed collaboratively by the Patient Information Committee of the North American Neuro-Ophthalmology Society. This has been written by neuro-ophthalmologists and has been edited, updated, and peer-reviewed by multiple neuro-ophthalmologists. The views expressed in this brochure are of the contributors and not their employers or other organizations. Please note we have made every effort to ensure the content of this is correct at time of publication, but remember that information about the condition and drugs may change. Major revisions are performed on a periodic basis.
This information is produced and made available “as is” without warranty and for informational and educational purposes only and do not constitute, and should not be used as a substitute for, medical advice, diagnosis, or treatment. Patients and other members of the general public should always seek the advice of a physician or other qualified healthcare professional regarding personal health or medical conditions.









_200x72.png)