QUICK LINKS: Practice Support Tools | Patients | Find a Neuro-Ophthalmologist | NOVEL | YONO Portal | Our Journal | Fellowships
Idiopathic Intracranial Hypertension/Pseudotumor Cerebri
Patients: Download as PDF
Clinicians: Download as PDF
What is idiopathic intracranial hypertension/pseudotumor cerebri?
Idiopathic intracranial hypertension (IIH), also called pseudotumor cerebri, is a condition in which there is high pressure in the fluid surrounding your brain, spinal cord and optic nerves. This can cause headaches and problems with vision. Although the cause(s) of the condition is not fully understood (the definition of “idiopathic”), we know much about the condition itself.
Do I have a tumor?
Patients with pseudotumor cerebri do not have a tumor. A brain tumor may also cause increased intracranial pressure, which is why this condition is called “pseudotumor”: it can cause symptoms like a real tumor, but the tests do not show any tumors (pseudo- means “false,” so pseudotumor means “false tumor”).
Who can get IIH?
IIH can affect anyone, but is more common in women (90%) than men. It is more common in teenagers and young women but can affect people of any age. It is much more common in those who are overweight, obese or who have had a recent substantial weight gain. Children who have not yet reached puberty can rarely get IIH. In these children, IIH occurs nearly equally in boys and girls and occurs in those who are not overweight.
What causes IIH?
We do not know what causes IIH. However, there is a clear association with being overweight or obese. Certainly, not all overweight or obese people develop this condition. This likely means that there are unique features that predispose some people to develop IIH that we have yet to discover. Medical studies have shown that recent weight gain can cause IIH, and that weight loss alone can achieve remission in most cases. There is ongoing research into the cause/causes of IIH. Certain medications increase a person’s chance of having IIH. These mostly include tetracycline antibiotics (e.g., minocycline, doxycycline), high doses of vitamin A and retinoids, so these should be discontinued and avoided in the future by people with this diagnosis. Growth hormone can rarely lead to IIH. Hormonal contraceptives (oral and implants) have not been convincingly shown to cause IIH and should not necessarily be discontinued in IIH patients.
How does IIH affect me?
Not everyone will develop all the symptoms of IIH. The most common symptoms of IIH include:
- Headaches
- Headache is the most common symptom, although not everybody with IIH has headaches. These headaches are often worse upon awakening or lying down.
- Brief visual changes such as dimming, blurring or graying of vision
- These changes only last for a few seconds (often with rising up after bending, stooping or lying down).
- Some patients notice blind spots to the side of their vision in each eye.
- Sounds of a whooshing heartbeat-like noise in the ears (pulsatile or pulse-synchronous tinnitus)
- Neck pain
Less common symptoms include:
- Double vision
- Nerve or back pain
- Nausea
In severe cases, IIH can cause severe peripheral vision loss and blurred central vision. If severe cases are left untreated, there is a high risk of permanent disabling loss of vision.
How is IIH diagnosed?
There are three important steps that must be completed in order to diagnose IIH:
- A complete eye exam must be performed, including special tests on your visual field and looking at the back of your eye (usually with pupil dilation) to look for swelling of the optic nerves caused by high pressure in the brain (papilledema).
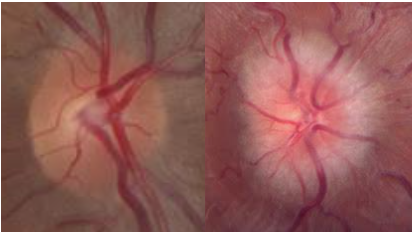
Courtesy of Dr. Valerie Biousse, M.D.
Normal optic nerve (left) and papilledema (right). The normal optic nerve looks like a flat pink-orange-yellow disc. In papilledema, the edges of the disc become blurred and fuzzy, and the entire disc eventually swells.
- Brain scans, in particular magnetic resonance imaging (MRI), usually including vein imaging (MRV), must show that there is no tumor, blood clot in the veins, or other cause for the suspected high pressure. Occasionally, if a patient cannot undergo an MRI, a CT (computed tomography) scan may be performed. Sometimes the brain scan report will say that there is flattening of the pituitary gland, extra fluid around the optic nerves, or narrowing of major veins inside the skull that suggest IIH. These can be useful clues for your doctor to diagnose IIH but cannot replace a lumbar puncture (spinal tap) to check the pressure of the spinal fluid.
- A lumbar puncture must be performed to confirm a high pressure and normal spinal fluid (CSF). The lumbar puncture must be performed with you relaxed and lying on your side with your legs straight, or in the prone position (on your belly) when done under radiographic guidance (fluoroscopy) for the reading to be accurate. Your doctor will review the risks and benefits of a lumbar puncture with you. A lumbar puncture is generally quite safe, but a temporary worsening of headache may rarely occur.
Why do I need to see a neuro-ophthalmologist? What is the role of other specialists in my care?
- Neuro-ophthalmologists are the experts with the most experience and knowledge about IIH. Though many neurologists and ophthalmologists may also see and manage people with IIH, neuro-ophthalmologists receive specific training to help take care of all forms of IIH. Many specialists may be involved in your treatment:
- Neuro-ophthalmologists evaluate and guide the medical and/or surgical treatment.
- Neuro-ophthalmologists or ophthalmologists monitor your vision by looking inside the eyes (often with pupil dilation), and performing visual field testing, photographs and/or a special imaging test called optical coherence tomography (OCT). Some ophthalmologists or neuro-ophthalmologists are specifically trained to perform optic nerve surgery, which may be one of several alternatives for management of severe cases of IIH.
- Neurologists may help coordinate the testing for diagnosing IIH and help treat headaches.
- Neurosurgeons may be involved if surgery (CSF shunting) is necessary to control the high pressure. Alternatively, specially trained neurosurgeons, neurologists, or interventional neuroradiologists may place a stent in one of the narrowed veins inside the skull in some cases that do not respond well to medications and weight loss.
How is IIH treated?
Most people with IIH are treated with medications and weight loss. Less than 1 out of 10 people (< 10%) with IIH will require surgical treatment.
Relatively few people become blind from IIH and most people recover if they are treated early. Surgery is needed if medical treatment and weight loss do not stop the visual loss. In very rare cases, blindness may occur even with correctly administered medications and surgery.
Main treatments of IIH
Do I need treatment?
If you do not have significant headaches or vision loss, no treatment may be necessary, although weight reduction is always a good idea to prevent the disease from worsening. The decision to treat or not treat is based on the clarity of your vision (visual acuity), peripheral vision (visual fields), presence of papilledema, and whether or not you have headaches or other symptoms.
Weight loss is hard to do. How much weight do I need to lose?
Weight loss can be a sensitive issue for both the doctor and the patient. Weight loss is difficult to achieve and maintaining a lower weight long-term is challenging. Almost all people with IIH are overweight, and weight loss can be a very effective component of treatment. Weight reduction programs that include increasing physical activity and a diet low in sodium have been shown to be effective in treating IIH. A good initial goal is losing 6-10% of your starting weight; for example, someone with a starting weight of 250 lbs (113 kg) would have an initial target weight loss of 16-25 lbs (7.3-11.3 kg). In some cases, weight management (bariatric) surgery may be helpful.
What medications are used for treating IIH?
Acetazolamide (Diamox) is the most common medication used for treating IIH. It is thought to lower pressure inside the skull by reducing fluid (CSF) production. Research shows that acetazolamide significantly improves vision, papilledema, quality of life and CSF pressure.
Common side-effects of acetazolamide include:
- Tingling of fingers and palms, toes and soles
- Decreased appetite
- Metallic taste when drinking fizzy drinks (carbonated beverages)
- Tiredness (fatigue)
- Kidney stones may occur in rare cases (2-3%)
If you are not able to take acetazolamide, your doctor may prescribe another medication called topiramate (Topamax) which may help the headache and also assists with weight loss. Side effects of topiramate can include mild slowing of thought processing. Furosemide and methazolamide are alternative medications that are sometimes used to treat IIH in patients who do not tolerate acetazolamide or topiramate.
What medications help for headache in IIH?
There are no medications specifically designed for IIH-related headaches, although many neurologists specifically use topiramate because it may also lower pressure inside the skull and may act as an appetite-suppressant. Over-the-counter analgesics such as non-steroidal anti-inflammatory drugs (NSAIDs) and/or migraine medications may be helpful if you have headaches even after the IIH treatment is successful in lowering the intracranial pressure and resolving the papilledema.
Using pain medications >2-3 days per week for more than a few months can make you dependent on the medications, so that when you don’t take the pain medications you get a withdrawal headache (medication-overuse headache). This is a background daily headache that may be confused with high pressure and can make the severe headaches worse. Stopping these medications is helpful. Consulting with a neurologist may be useful if headaches are a persistent concern.
Surgical Treatments
Surgery is recommended when vision is getting worse from high pressure despite aggressive treatment with medications and best efforts at weight loss. Because surgery has small but potentially dangerous risks to your life and/or vision, surgery for IIH is usually not recommended when your vision is good. The goal of surgery is to release pressure around the optic nerves. There are three main types:
-
Shunt surgery: a neurosurgeon places one end of a flexible tube into one of the normal fluid-filled spaces in your brain (ventricle) or into your lower (lumbar) spinal canal and the other end into another part of your body, such as your abdomen (peritoneum). This allows the fluid under high pressure in the head a way to escape.
-
Venous stenting: A specially-trained neurovascular surgeon inserts a device that holds open a vein inside your skull that drains blood from the brain. If a patient has a vein narrowing inside the skull that is restricting blood flow, opening it more fully with a stent can lower the pressure inside the skull. It is a newer technique for lowering pressure inside the skull. Specialists are still determining when it is best to use venous sinus stent placement in the treatment of IIH. You will need to be on a blood thinner for several months after the procedure and thus venous stenting is not a good option for patients who are pregnant.
-
Optic nerve sheath fenestration: an orbital or neuro-ophthalmic surgeon creates a small window in the lining (sheath) around your optic nerve to allow the fluid to drain behind your eye, which lowers the pressure on the front of the optic nerve and helps optic nerve swelling improve.
When will the IIH go away? Can the IIH come back?
IIH may resolve over months to years or it may be a lifelong medical problem. IIH can return, and is often linked to regaining weight (even just 6-10% of body weight). If you become pregnant in the future, inform your neuro-ophthalmologist, as you may require closer follow up during your pregnancy. However, IIH during pregnancy does not require a Cesarean section.
What changes in symptoms should I pay attention to after being diagnosed with IIH?
You should let your neuro-ophthalmologist know about any changes in symptoms such as worsening headache. You should report changes in vision immediately since that could indicate worsening optic nerve swelling, which could lead to permanent loss of vision if left untreated.
Will I need another spinal tap in the future?
Generally not, unless there is a new problem or if it is unclear whether the pressure in your head is still high and a repeat measurement would change how you are treated. IIH is now only rarely treated with multiple spinal taps.
Does IIH run in families?
IIH rarely runs in some families (approximately 5%).
Additional Reading/Resources
Other Websites
- National Eye Institute
- American Academy of Ophthalmology
- Mayo Clinic Website
Support Groups
- Links to two major support groups are listed below.
Copyright © 2023. North American Neuro-Ophthalmology Society. All rights reserved.
This information was developed collaboratively by the Patient Information Committee of the North American Neuro-Ophthalmology Society. This has been written by neuro-ophthalmologists and has been edited, updated, and peer-reviewed by multiple neuro-ophthalmologists. The views expressed in this brochure are of the contributors and not their employers or other organizations. Please note we have made every effort to ensure the content of this is correct at time of publication, but remember that information about the condition and drugs may change. Major revisions are performed on a periodic basis.
This information is produced and made available “as is” without warranty and for informational and educational purposes only and do not constitute, and should not be used as a substitute for, medical advice, diagnosis, or treatment. Patients and other members of the general public should always seek the advice of a physician or other qualified healthcare professional regarding personal health or medical conditions.









_200x72.png)