QUICK LINKS: Practice Support Tools | Patients | Find a Neuro-Ophthalmologist | NOVEL | YONO Portal | Our Journal | Fellowships
Giant Cell Arteritis
Patients: Download as PDF
Clinicians: Download as PDF
What is Giant Cell Arteritis (GCA)?
Giant cell arteritis is an inflammatory condition that can cause vision loss, double vision, fever, new persistent headaches, scalp tenderness, and jaw pain with chewing. GCA is caused by inflammation of blood vessels, primarily in the head and neck. Sometimes called “temporal arteritis,” GCA frequently affects blood vessels in the temples, causing headaches. GCA can affect other blood vessels in the body, and in severe cases, cause heart attack or stroke.
GCA almost exclusively affects people older than the age of 50. The average age of onset is 70 years. GCA affects both men and women and can occur in any race or ethnicity. The cause of GCA is unknown.
How Does Giant Cell Arteritis Affect My Vision?
Inflammation in GCA causes blood vessel narrowing, which can affect blood supply to the optic nerve or retina and cause permanent vision loss. Vision loss in one or both eyes occurs in 20-50% of patients. Approximately 1/3 of patients who lose vision from GCA experience transient vision loss in one eye 7-10 days prior to the permanent vision loss. If not recognized and treated promptly, the second eye will lose vision within 7-10 days in 70% of cases. Vision loss is typically severe and almost always irreversible, even with treatment. For this reason, early diagnosis and prompt treatment are imperative. Intermittent or sustained double vision can also be a warning sign of impending visual loss.
What are Other Symptoms of Giant Cell Arteritis?
The most common initial GCA symptom is a new persistent headache, which is present in 40-90% of patients. Scalp tenderness is also common and often noticed when brushing or washing hair, or sleeping on one side of the head. Less common, but important symptoms include pain and fatigue in the jaw, ear, tongue, throat, or neck while chewing or swallowing, especially after doing so for a few minutes. These symptoms, called jaw claudication, are very concerning for GCA and should be taken very seriously.
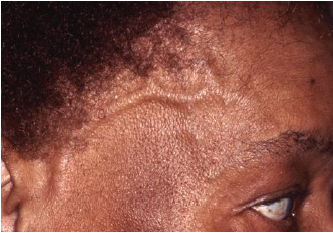
Many people with GCA have only nonspecific symptoms such as fatigue, generalized malaise, fever, loss of appetite, unintentional weight loss or decreased appetite. Other neurological symptoms include numbness, tingling, hearing loss, or dizziness. Severe cases can result in heart attack, stroke, or kidney damage. Thickened and inflamed blood vessels in the temple may even be visible, as shown in the figure below.
Why Do I Need to See a Neuro-ophthalmologist?
Neuro-ophthalmologists are experts on GCA, especially for patients with vision loss. While many specialists will likely be involved in your care, neuro-ophthalmologists receive specific training to diagnose and manage patients with vision loss, double vision, and other visual symptoms associated with GCA.
- A neuro-ophthalmologist diagnoses GCA, monitors your visual status, and guides treatment based on your eye exam, symptoms, and lab values.
- A rheumatologist is an expert in inflammatory disease and the use of anti-inflammatory medications. They often co-manage the disease alongside the neuro-ophthalmologist in patients with vision loss. The rheumatologist is frequently the main physician who manages GCA.
- An internal medicine or family medicine physician monitors for potential treatment side effects and evaluates for GCA elsewhere in the body, especially the aorta.
Your neuro-ophthalmologist will monitor your central and peripheral vision as well as your color vision, eye movements, and general eye health. They will perform a dilated eye exam and a visual field test to map your peripheral vision. Additional imaging tests may include retinal photographs, optical coherence tomography (OCT), and fluorescein angiography (FA).
How is Giant Cell Arteritis Diagnosed?
If your doctor suspects you have GCA, you will need urgent blood testing to screen for inflammation including Erythrocyte Sedimentation Rate (ESR), C-reactive protein (CRP), and Complete Blood Count (CBC). People with normal blood tests are much less likely to have GCA, although there are exceptions and you may still require further investigations and treatment.
If your doctor thinks you have GCA, you will be started on high dose steroids, either orally (i.e., prednisone) or intravenously (methylprednisolone). These medicines control inflammation and are not the same as the anabolic steroids that athletes sometimes take. Your doctor will also arrange for a temporal artery biopsy within 7-10 days.
A temporal artery biopsy is required for definitive diagnosis of giant cell arteritis. This is typically an outpatient procedure that takes less than an hour and typically does not require general anesthesia. A small segment of artery located just beneath the skin on your temple is removed and sent to a pathologist to examine under a microscope. The biopsy may be done on one or both sides. If you are taking a blood thinner, it may need to be stopped a few days before the procedure. It is uncommon, but possible, for a biopsy to be negative in patients with GCA. If your doctor still believes you have a high risk for GCA despite a negative biopsy, they may still recommend continued steroid treatment.
How is Giant Cell Arteritis Treated?
GCA is primarily treated with high-dose steroids. The disease is typically active for 1-2 years, but in some cases, can last up to 10+ years. Therefore, people with GCA may take steroids for a long time. Headache and pain usually improve within 24-72 hours of starting treatment. Unfortunately, vision does not typically improve, and may even worsen despite treatment. The goal of prompt treatment is to prevent further visual loss and other serious complications of GCA like stroke and heart attack.
Once you begin steroid treatment, your doctor will continue to check blood work (ESR and CRP) and follow your symptoms for several months to years. Your doctor will gradually lower your steroid dose as the inflammation in your body improves. Most patients eventually stop steroids completely.
In 2018, the FDA approved a medication called tocilizumab that, if taken in addition to steroids, can shorten the duration of steroid treatment in patients with GCA. The choice of long-term medication for GCA should be made in conjunction with your neuro-ophthalmologist, rheumatologist, internist, family practitioner, or a combination of these doctors.
What is My Prognosis?
With early treatment, GCA has a good prognosis for survival. Unfortunately, vision loss is typically permanent regardless of treatment. The goal of treatment is to avoid vision loss in the other eye, to limit worsening of vision, and to prevent damage to other organs.
Additional Resources:
- American Academy of Ophthalmology EyeWiki: http://eyewiki.org/Giant_Cell_Arteritis
- Vasculitis Foundation: https://www.vasculitisfoundation.org/education/forms/giant-cell-arteritis/
- American College of Rheumatology: http://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Giant-Cell-Arteritis
Support Groups:
- Vasculitis Foundation: https://www.vasculitisfoundation.org/support
- Facebook group for patients with giant cell arteritis: https://www.facebook.com/groups/661801073922595
Copyright © 2023. North American Neuro-Ophthalmology Society. All rights reserved.
This information was developed collaboratively by the Patient Information Committee of the North American Neuro-Ophthalmology Society. This has been written by neuro-ophthalmologists and has been edited, updated, and peer-reviewed by multiple neuro-ophthalmologists. The views expressed in this brochure are of the contributors and not their employers or other organizations. Please note we have made every effort to ensure the content of this is correct at time of publication, but remember that information about the condition and drugs may change. Major revisions are performed on a periodic basis.
This information is produced and made available “as is” without warranty and for informational and educational purposes only and do not constitute, and should not be used as a substitute for, medical advice, diagnosis, or treatment. Patients and other members of the general public should always seek the advice of a physician or other qualified healthcare professional regarding personal health or medical conditions.









_200x72.png)